And you may or may not know it!
| Quick Summary | |
|---|---|
| There is bad news | The incidence, prevalence and costs for type 2 diabetes are probably worse than we know. |
| There is good news | As an organization, it is important for you to know there are options that will have a positive impact on the incidence, prevalence and costs of type 2 diabetes. |
Type 2 diabetes is a problem on many levels. The employer level is one, particularly if you provide health insurance to your employees.
I will be focusing on the employer burden in this article in an effort to explain why type 2 diabetes is such a problem.
Descriptive statistics on type 2 diabetes
Before getting into the data, I need to define a few terms you may or may not be familiar with:
- Type 2 Diabetic: A person diagnosed with type 2 diabetes. The normal cutoff for diagnosis is a fasting blood sugar greater than 126 mg/dL.
- Pre-diabetic: A person with higher than normal fasting blood sugar but not high enough to be diagnosed as type 2 diabetic. A normal fasting blood sugar level is below 100 mg/dL. A pre-diabetic is someone with a blood sugar (at the time of testing and/or diagnosis) greater than 100 mg/dL but less than 126 mg/dL.
- Undiagnosed: This is someone that should be counted in one of the two categories above. They aren’t counted, however, because they haven’t been officially diagnosed by a medical professional.
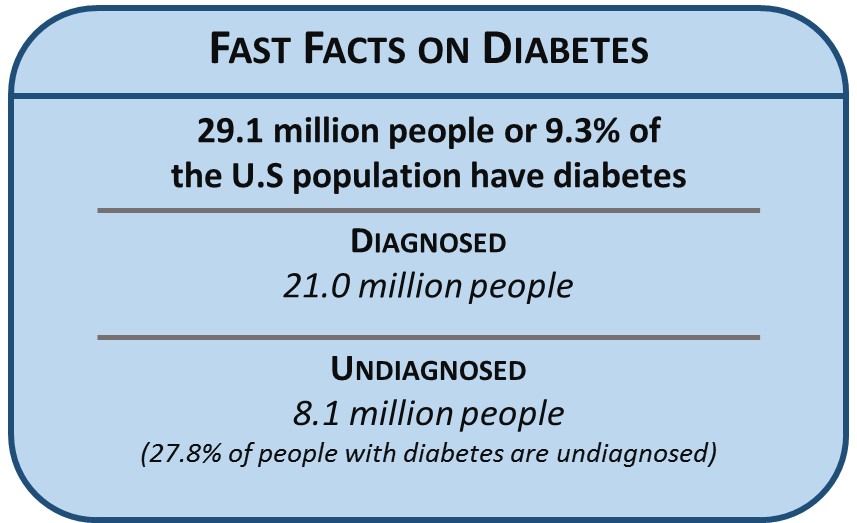
Data from the CDC and other health-related government agencies indicate that about 29.1 million Americans are either diagnosed or undiagnosed type 2 diabetics. Additionally, there are about 86 million Americans in the pre-diabetic category, which means a total of 115.1 million Americans have some form of type 2 diabetes.
What about costs?
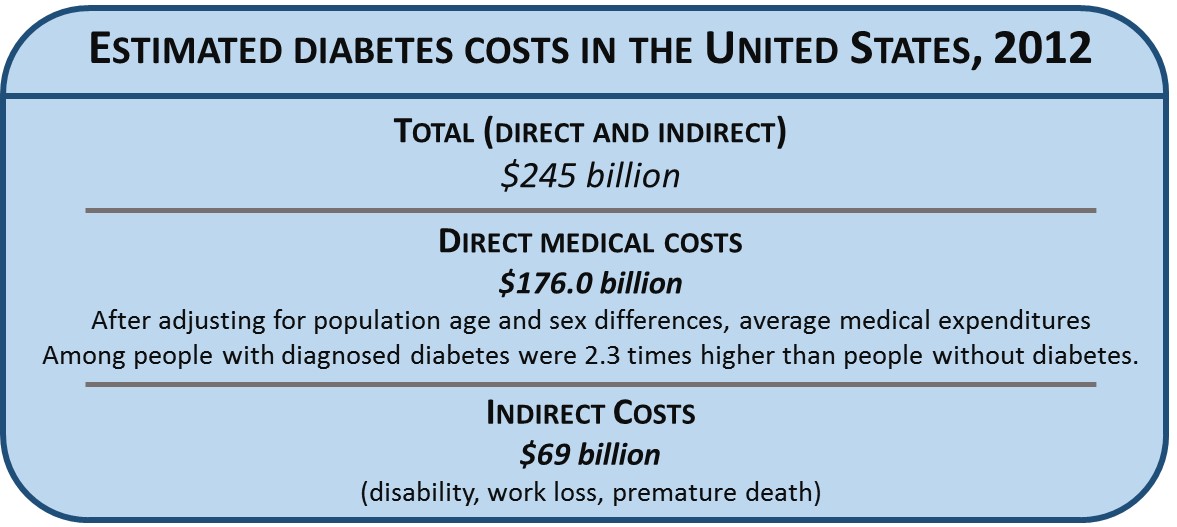
The same report states the total direct and indirect costs for type 2 diabetes was $245B in 2012 or about $2,200 per person (for the 115.1 million with some form of type 2 diabetes). Of this total, direct costs were $176 billion and indirect costs accounted for the rest.
In terms of where costs are going, they will increase (they always do, so it is a big limb I’m going out on). The cost of doing business never goes down. So the cost to treat a type 2 diabetic (or a person with any condition) will never be cheaper than it is today.
More specifically, the costs associated with type 2 diabetes are high because the condition has a negative impact on virtually every system in the body. This negative impact significantly increases risk for nearly every other chronic disease and/or condition. For example, those with type 2 diabetes have a 60% greater risk of dementia than those without diabetes. Additionally, epidemiological studies indicate type 2 diabetics have approximately twice the risk of developing liver or pancreatic cancer than non-diabetics. The “For example” list could go on almost without end and I haven’t mentioned a whole host of comorbidities, such as neuropathy, nephropathy, vision problems and more.
For many reasons, the cost of care for a type 2 diabetic is high.
And it’s probably actually worse!
There is a progression of tests an individual goes through before being diagnosed as a type 2 diabetic. This progression doesn’t get started until he/she consistently has a blood sugar reading of greater than 100 mg/dL. This is a problem on at least two levels.
First, not everyone at risk will have their blood sugar tested. Further, if they get their blood sugar tested (as is often the case for an employer’s incentivized “wellness” program) the typical response to those with elevated blood sugar is to refer them to their physician. Follow up is generally left to the discretion of the individual, unless there is sever hyperglycemia.
Second, a simple finger stick to measure blood sugar lacks sensitivity and specificity to make an accurate judgment based on the results (false positives and false negatives). This, incidentally, may play a role in why follow up isn’t pursued vigorously.
A recent report in the Journal of the American Medical Association (JAMA) sheds light on why the problem of type 2 diabetes is likely worse than what we think (or know). By including a more appropriate test and using the same datasets, the authors concluded that 52.4% of the population has some form of diabetes.
This table summarizes the differences in the two reports.
| The CDC vs JAMA reports | ||
|---|---|---|
| CDC | JAMA | |
| Total Diabetes (millions) | 115.1 | 129.3 |
| Pre-diabetics (millions) | 86.0 | 110.8 |
| Total Costs | $245.0B | $284.5B |
| 5-year projected costs | $343.0B | $398.3B |
Note how the data from the JAMA report are much higher across the board when compared to the CDC report. This is significant and as noted earlier, the authors of the JAMA report used the same dataset. However, they included HbA1c as a criterion, where the CDC report did not. The publication of the JAMA report lead us to write a Call to Action last year.
Just a $40 billion difference!
From the CDC report, the cost per person with diabetes was approximately $2,200 per year. If we apply that to the JAMA report, the true cost is closer to $284.5 billion – just a $40 billion difference!
Plus the cost increase in the 5-year assessment period for the CDC data was 40%. If we apply this to the JAMA report, projected costs are nearly $400 billion. In just a few short years, we will be spending nearly a half trillion on type 2 diabetes alone.
From the abstract of the JAMA article:
The incidence of type 2 diabetes …increased significantly in every age group, in both sexes, in every racial/ethnic group, by all education levels, and in all poverty income ratio tertiles.
These across the board increases are sobering. They mean, essentially, that more than 1 in 2 adults (52.4%) over the age of 20 have some form of type 2 diabetes.
Kicking the can down the road
As bad as these numbers sound, the reality will likely be worse. One reason is our current approach to treatment, which is symptom-based. Type 2 diabetes is a problem with insulin resistance. Elevated blood sugar is a symptom of insulin resistance, yet the current treatment approach is targeted at elevated blood sugar. In spite of mounting evidence that we can improve insulin sensitivity, the current symptom-centric approach guarantees two things:
- From a population perspective, the state of insulin sensitivity will not improve. In fact, insulin sensitivity will likely worsen.
- For those with pre-diabetes, 25% will be full-blown type 2 diabetic within 5 years.
Given these two guarantees, coupled with the sobering statistics from the JAMA report, it is easy to conclude this will likely be worse than the projections.
So what about costs at your company?
I don’t need to state the obvious because you know healthcare costs are rising and a concern. This is the question that needs to be asked:
What effective and measurable strategies can employers deploy?
There are many programs and solutions offered by carriers, vendors, and benefits consultants in the marketplace. The problem is that most have little to no significant impact on your total spend. Additionally, most lack the ability to effectively measure results. Whether you use specific “wellness” programs, technology, gadgets, etc… or not, if you do nothing to change incidence and prevalence of type 2 diabetes in your workforce, the impact of cost control will be small.
So what if you have 1,000 employees?
Of your workforce, more than 500 will have some form of type 2 diabetes. The diagnosed and undiagnosed will account for almost 200 of these and the rest will be pre-diabetics (If you are thinking that the annual Health Risk Appraisal showed that you were well below these estimates, great. But you might want to reconsider. It’s likely that fasting blood sugar was used instead of HbA1c and there are issues with that, as discussed above).
These 500 employees will cost you about $1.1 million in healthcare expenses alone ($2,200 cost to treat X 500 employees). That’s a lot of money, even for massive companies like Microsoft, Apple and Exxon.
Sure, you can do things to control costs of prescription medications – generics, mail order, recommendations from a PBM, etc… But these are the margin things – 1 or 2% of $1.1 million is ok but not enough.
You might also consider a customized wellness plan (or maybe have). This is the type of thing they are supposed to address. The problem is, they don’t.
Good News, Finally!
To stop diabetes from killing your company, you have to stop operating in the margins. This is the only way you can bend the curve because the small cost control measures have zero impact on the incidence and prevalence of type 2 diabetes.
How do you do that?
Find something that turns the whole thing upside down! And you have to look. The right program for you and/or your company is out there. But you likely won’t find what you need from your broker, insurance provider or program administrator, because most of what they offer does not address insulin sensitivity.
Talk with a trusted adviser – your HR consultant, financial analyst or business leader. Some brokers can be helpful, but they are the exception not the rule.
At the Health Performance Institute, we offer programs that help improve insulin sensitivity in their employees. If you have questions or would like to talk with us, fill out our online form or email me directly.
If the trend in your company for type 2 diabetes (or any chronic condition) is going up and not down, the time to act is now. Otherwise, you are guaranteed to face increasing healthcare costs in the future.
You have options to bend the curve and change the status quo. But you must act now to change the future of your company!
A special Thank You to the following
This article could not have been written without their help and critical feedback. They did this in spite of their busy schedules. So for that, I am very appreciative.
| Name and Contact Info | Title | Company | |
|---|---|---|---|
 |
Hang Bower Bio @ hrQ Phone: 713-999-9380 |
VP & Managing Director |
|
 |
Juliet Breeze, MD Phone: 281-201-0657 Find a location |
President/CEO | Urgent Care |
 |
Brian Frank Phone: 713-490-4529 LinkedIn bio |
Consultant, Employee Benefits |

As someone over 50, and in the healthcare industry for 20 years, I can concur that Type 2’s are under diagnosed and under treated. My father was always considered a “borderline type 2”, but was religious in taking his meds. Many borderline men, simply view being borderline as being ok, and don’t monitor their situation or go back for further treatment, which end up being a bigger cost both physically and financially.
Excellent article!
Hi Rick, thank you and I appreciate the compliment! What your dad went through is part of the problem. People in his situation don’t hear from their healthcare professional that taking medication isn’t enough. And as you correctly state, they end up as type 2 diabetic – at greater financial and health cost.
Pingback: Webinar: Why Wellness Fails April 2016 – The Health Performance Institute
Pingback: Why Wellness Fails – The Health Performance Institute